What we do
About our project
This large project took more than 2 years to complete, and was funded by the Dutch government as part of the process to create a clinical management guideline. The guideline is due to be published in Dutch later in 2020. Once this in completed you will be able to access the guideline here.
Our aim was to evaluate the comparative effectiveness of all available treatments for Achilles tendinopathy in a regularly updated (“living”) systematic review using a network meta-analysis. We plan to keep updating this review every 2 years. Future results will be posted here every 2 years. When there are clinically relevant changes that impact clinical decision-making, we will plan to publish a new update as scientific article.
Methods of our project
Patients with Achilles tendinopathy assisted in the design of the study. They were involved in focus interviews, and a survey among patients was used to identify relevant outcomes. The Victorian Institute of Sport Assessment-Achilles (VISA-A) questionnaire was defined as primary outcome of this review, as the items measured in this questionnaire were regarded as most important for patients.
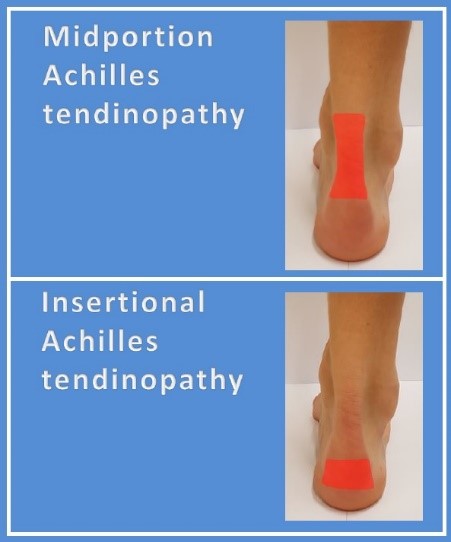
This living systematic review with network meta-analysis was prospectively registered. State-of-the-art methodology and guidelines were followed in the design phase. Multiple databases were searched up to February 2019. Large randomised clinical trials examining the effectiveness of any treatment in patients with both insertional and/or midportion Achilles tendinopathy were eligible. A number of treatment classes were pre-defined, which was based on the assumption that some treatments have a similar effect because of a comparable working mechanism. Reviewers independently extracted data and assessed risk of bias. Network plots were constructed using Stata software to visualise all head-to-head comparisons. Treatment-level and class-level models were fitted in a Bayesian framework using specific simulations. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to appraise the quality of evidence.
Results:
We identified 5154 potentially relevant publications, of which 170 articles were screened in the full-text analysis. 29 trials (n=1640 patients) were included investigating 42 different treatments. These are visualised in the network plots. 22 trials (76%) were at high risk of bias and 7 (24%) had some concerns. Most trials included patients with midportion tendinopathy (86%). No NMA could be performed for insertional Achilles tendinopathy.

These tables show comparative treatment class effects expressed with a mean difference for the VISA-A score at 3 months (A) and at 12 months (B) in patients with midportion Achilles tendinopathy. Mean differences on the VISA-A score with their 95% credible intervals from the network meta-analysis. For any cell, a negative mean difference favours the upper-left treatment, and a positive mean difference favours the lower-right treatment. Comparative treatment class effect differences are shown in bold.

Treatment class rankings from the network meta-analysis for the VISA-A score at 3 months in patients with midportion Achilles tendinopathy. Any treatment class seemed superior to wait-and-see for midportion Achilles tendinopathy at 3 months (very low-low certainty of evidence).

Treatment class rankings from the network meta-analysis for the VISA-A score at 12 months in patients with midportion Achilles tendinopathy [LINK naar treatment class rankings 12 months]. Exercise therapy, exercise+injection therapy, and exercise+night splint therapy, were all comparable to injection therapy for midportion tendinopathy (very low-low certainty).
Conclusions:
In this living systematic review and network meta-analysis:
- None of the trials were at low risk of bias
- All evaluated treatments had large uncertainty in the estimates
- Active treatment classes seemed to have patient-important benefits (mean difference exceeded the minimum important difference of 15 points on the VISA-A score) at 3 months compared to wait-and-see
- For two classes (acupuncture therapy and shockwave therapy combined with exercise therapy), the credible intervals exceeded the minimum important difference of 15 points on the VISA-A score at 3 months. However, these results were based on two small at high risk of bias. There were no estimates for effectiveness of wait-and-see at 12 months
- The effectiveness of most active treatments in the long term is uncertain. At 12 months, there was no difference between exercise therapy, injection therapies and combined therapies
Clinical implications:
- Wait-and-see should not be recommended as strategy for Achilles tendinopathy
- Active treatments had overlapping comparative effects, leaving uncertainty about which treatment is best for Achilles tendinopathy
- Shared decision making between healthcare providers and patients therefore plays an important role in the choice of treatments. Preferences of patients, safety profile, availability of the treatment, and costs should be taken into account in this clinical decision-making process
- Clinicians should consider starting with calf-muscle exercise therapy as initial treatment. Calf-muscle exercise therapy may be easy to prescribe because it is easy to instruct, it is suggested to be cheap, is available everywhere and has a low risk of harm
Funds & Grants
Collaborations
External collaborations
- Patients who suffered self- reported Achilles tendinopathy
- Aspetar Orthopaedic and Sports Medicine Hospital
- Aalborg University, Centre for General Practice, Aalborg, Denmark
- Karolinska Institute, Division of Physiotherapy, Stockholm, Sweden
- Bristol Medical School, Population Health Sciences, Bristol, United Kingdom
Publications
The results of the review have been published in the highly rated “British Journal of Sports Medicine” available open access.
Our team
M. Winters
A. Weir
C.L. Ardern
N.J. Welton
D.M. Caldwell
J.A.N. Verhaar
R.J. de Vos
