With the establishment of the Transplantation Institute, we are bringing together the knowledge and expertise of the various specialties, because together, we know more and can do more. With hepatologists, nephrologists, cardiologists, pulmonologists, anesthesiologists, intensivists, surgeons and rehabilitation physicians, we draw up the highest achievable transplant and rehabilitation pathway This pathway is created in consultation with the patient; our aim is that every patient we treat receives the highest level of care possible.
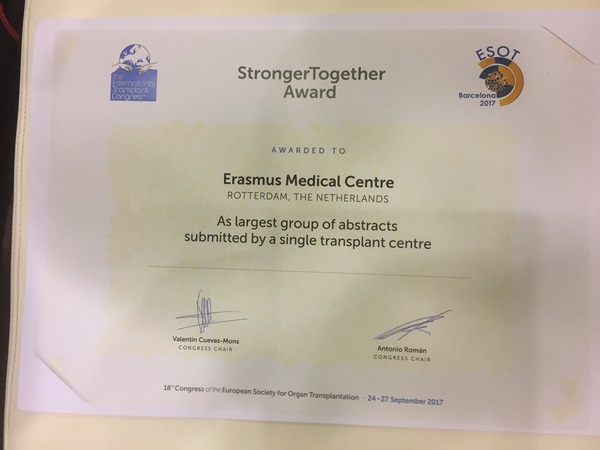
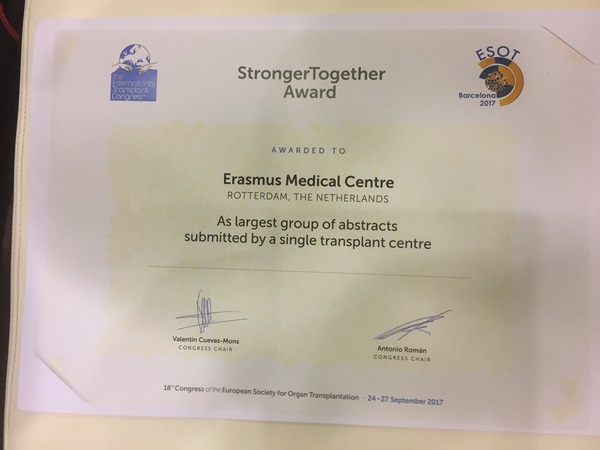
'Stronger Together' Award
In both 2017 and 2019, we received the 'Stronger Together Award' from the European Society for Organ Transplantation (ESOT)'. An appreciation for the strongest scientific collaboration of different organ transplant programs within a center. And we are proud of that!
And if necessary, we go one step further. We have the latest knowledge and techniques, but are always looking for new possibilities. What is still possible from a medical point of view, even though there seems to be few options left? That is our motivation to make a difference.
We think in terms of opportunities and possibilities. We demonstrate this best with examples:
- A donor kidney with a cyst in it.. It would be a waste to decline an organ for this. Can the cyst be removed before transplantation? We do everything we can to not reject any donor organ.
- A liver with a flaw in it. Due to a congenital defect, the liver cannot process certain proteins properly. One patient may not be able to live with this, but another may be better off with this liver than with his own sick liver. Affected organs can still be valuable.
- An overweight patient. That can be a risk for transplantation but still, we look at the possibilities. We look not only at the BMI-score, but also at someone's physical characteristics. And look for alternatives, such as the most appropriate surgical technique.
- Too old? We don't say that easily. We have a 91-year-old man who altruistically donated his kidney. And, our oldest kidney recipient was an 85-year-old woman. She successfully received a new kidney.
- Lung transplants also no longer have ‘hard’ age limits. We look at biological fitness of our patients.
- When blood vessels are not suitable enough for transplantation, we make them suitable. For example, by constructing a bypass.
- Also special: because of a congenital defect, a young man could not undergo general anesthesia. We transplanted him under local anesthesia.
- Sometimes we transplant a person two or even more times. For example, when a transplant loses its function. And very occasionally, we do it 7 times (Story in Dutch only). A 34-year-old man set a record with this.
- Does a patient have little chance of a direct kidney supply? Then we first remove the barriers of blood groups or tissue proteins. Then we can still transplant.
- Is a patients’ heart failure so severe that he is in danger of dying before a donor heart is available? Then we'll see if we can keep him alive with a mechanical support heart.
- Is there no surgical team available because a transplantation is already in progress? Then we will arrange a second team, because we do not allow donor organs to go to waste.
- Patients with irreversible lung damage from COVID-19 infection sometimes survive only by lung transplantation. We were the first in the Netherlands to perform successful lung transplants in these patients.
- We also transplant patients who are in the intensive care unit (ICU) with lung failure. Here, the ICU bridges the time until transplantation. We help them breathe and use the heart-lung machine if necessary. The results of these transplants are similar to those of transplanted patients who were not in the ICU.
To be able to do even more for our patients, we are constantly looking for new possibilities. At the moment, for example, we are conducting the following studies:
- In 4 studies we are investigating the effect of corona vaccination on kidney patients. Little is known about this. This is important information, because for kidney patients an infection with coronavirus is more dangerous, and vaccination is of vital importance.
- We are investigating whether we can use an ‘electronic nose’ to detect complications after transplantation. These include rejection of a donor organ, infections or diabetes. We do this with heart and lung transplant patients. This is a good example of the collaboration within our institute.
- We are looking for the best way to suppress the rejection of an organ, using medications that cause as few side effects as possible for each patient. We aim to have customized medications for everyone.
- We want to gain more insight into short- and long-term organ rejection. Our kidney transplant program already has a lot of experience in this area. We are transferring that knowledge to the other organ transplant programs.
- We are studying the risks of transplantation in people who are obese, have high blood pressure or impaired kidney function. How can we help them?
- We provided tailored care to young children and teenagers who underwent heart or kidney transplants. How are they doing now? What can we learn from them? What could be improved?
- We would like to know how daily medication use can be improved, so that we can be confident that medications are always taken. How can we make it easier for our patients? What mental factors play a role?
- Better fitness before transplantation gives less chance of complications during and after surgery. With online guidance programs (E-health), we improve the condition and resistance of the patient before transplantation, as well as the quality of life after transplantation.
- We are always looking for new drugs and therapies, such as when a transplant doesn't seem possible because of too many antibodies in the body, or because of a difference in blood groups.
- We want patients to live as long as possible with the best possible organ. That is why we are looking for more possibilities to improve the health and quality of a donor organ.