About O. (Odilia) Corneth MSc, PhD
Description of Research Line
Interstitial Lung Disease and Lymphocyte Signaling
Research in my group focuses on the role of B and T lymphocytes in chronic inflammatory diseases of the lung, such as interstitial lung disease (ILD) and sarcoidosis. I am interested in the role of B cell receptor signaling molecules, particularly Bruton’s tyrosine kinase (BTK), and how aberrant signaling can affect B-T cell interaction and the activation status of naïve B cells. Over the past few years, I have studied the role of B cells and BTK in idiopathic pulmonary fibrosis as well as various autoimmune diseases such as Sjögren’s syndrome (SjS), rheumatoid arthritis (RA), ANCA-associated vasculitis and systemic sclerosis, which may be associated with ILD. To study these patients, we have fruitful collaborations with research groups in various university medical centers in the Netherlands. In sarcoidosis, we focus on the T cell compartment, both in patients and in mouse models based on aberrant expression of the negative regulator CTLA4 on the cell surface of Th17 cells and regulatory T cells.
Education and career
After studying Medicine and Molecular Medicine at Erasmus University Rotterdam, she performed her PhD project at the Rheumatology Department of the Erasmus MC (supervision dr. Erik Lubberts; Prof. Rudi Hendriks, Prof. M. Hazes), studying Th17 cells in rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) patients. After obtaining her PhD in 2013, she moved to the Department of Pulmonary Medicine to study B cells, B-T cell interaction, B cell receptor signaling and in particular Bruton’s tyrosine kinase (BTK) in several autoimmune diseases.
Recent Publications
1. Miedema JR, de Jong LJ, Kahlmann V, Bergen IM, Broos CE, Wijsenbeek MS, Hendriks RW, Corneth OBJ. Increased proportions of circulating PD-1(+) CD4(+) memory T cells and PD-1(+) regulatory T cells associate with good response to prednisone in pulmonary sarcoidosis. Respir Res. 2024.
2. Neys SFH, Heutz JW, van Hulst JAC, Vink M, Bergen IM, de Jong PHP, Lubberts E, Hendriks RW, Corneth OBJ. Aberrant B cell receptor signaling in circulating naive and IgA(+) memory B cells from newly-diagnosed autoantibody-positive rheumatoid arthritis patients. J Autoimmun. 2024.
3. Miedema JR, de Jong LJ, van Uden D, Bergen IM, Kool M, Broos CE, Kahlmann V, Wijsenbeek MS, Hendriks RW, Corneth OBJ. Circulating T cells in sarcoidosis have an aberrantly activated phenotype that correlates with disease outcome. J Autoimmun. 2023.
4. Hendriks RW, Corneth OBJ. B Cell Signaling and Activation in Autoimmunity. Cells. 2023.
5. Neys SFH, Heukels P, van Hulst JAC, Rip J, Wijsenbeek MS, Hendriks RW, Corneth OBJ. Aberrant B Cell Receptor Signaling in Naive B Cells from Patients with Idiopathic Pulmonary Fibrosis. Cells. 2021.
6. Neys SFH, Rip J, Hendriks RW, Corneth OBJ. Bruton's Tyrosine Kinase Inhibition as an Emerging Therapy in Systemic Autoimmune Disease. Drugs. 2021.
7. Rip J, de Bruijn MJW, Neys SFH, Singh SP, Willar J, van Hulst JAC, Hendriks RW, Corneth OBJ. Bruton's tyrosine kinase inhibition induces rewiring of proximal and distal B-cell receptor signaling in mice. Eur J Immunol. 2021.
8. Rip J, de Bruijn MJW, Kaptein A, Hendriks RW, Corneth OBJ. Phosphoflow Protocol for Signaling Studies in Human and Murine B Cell Subpopulations. J Immunol. 2020.
Recent research findings
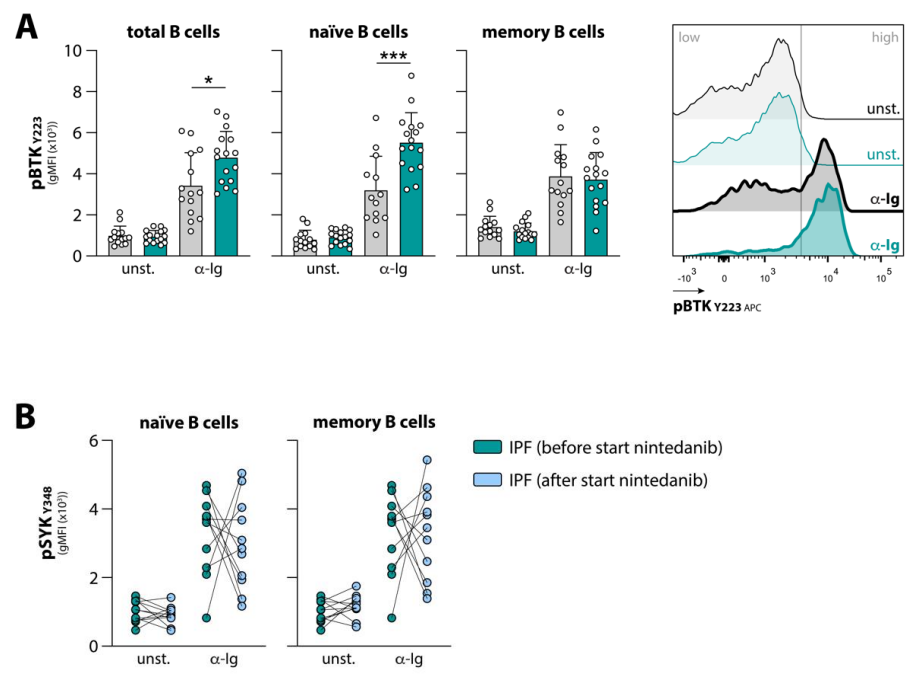
Previous studies in the lab have shown that mice overexpressing BTK specifically in B cells spontaneously develop an SLE/SjS-like autoimmune phenotype. We recently found that BTK protein levels in circulating B cells of autoimmune patients are increased, compared to healthy B cells. In active RA and SjS patients, these levels correlate with autoantibodies and in SjS with T cell infiltration in the affected organs. Furthermore, treatment of SjS patients with abatacept (CTLA4-Ig), which targets T cell co-stimulation, reduces BTK expression in their B cells to levels of healthy individuals, indicating that B-T cell interaction affects BTK in B cells and drives autoimmunity. We also studied B cells in IPF, a chronic and ultimately fatal disease in which an impaired healing response to recurrent micro-injuries is thought to lead to fibrosis. We showed that the response to BCR stimulation is enhanced in peripheral blood B cells from treatment-naïve patients with IPF. We observed increased anti-immunoglobulin-induced phosphorylation of BTK in naïve but not in memory B cells of patients with IPF. Interestingly, treatment of IPF patients with nintedanib, a tyrosine kinase inhibitor with mainly anti-fibrotic activity, induced substantial changes in BCR signalling.
Group members
PhD students: Lieke de Jong, Vicky Bogaard
Postdocs: Zahra Khalajzeyqami
Clinicians: Thomas Koudstaal (pulmonary fibrosis), Jelle Miedema (sarcoidosis), Merel Hellemons (long COVID)
